Frequently asked questions
About the negotiation
Broward Health hospitals, physicians and other clinicians and its other service locations have become out-of-network for all services as of July 1, 2025.
This means Broward Health could make you pay more for services.
All Broward Health hospitals, facilities, and hospital-based physicians have become out-of-network as of July 1, 2025.
Broward Health (North Broward Hospital District) and Florida Blue have entered numerous contract renewal negotiations during our longstanding relationship, and previously successfully reached agreement on new terms. We’ve worked hard to resolve this latest negotiation without any disruption to the care of our members, and will continue trying to reach an agreement even after July 1st — to get Broward Health back in our network
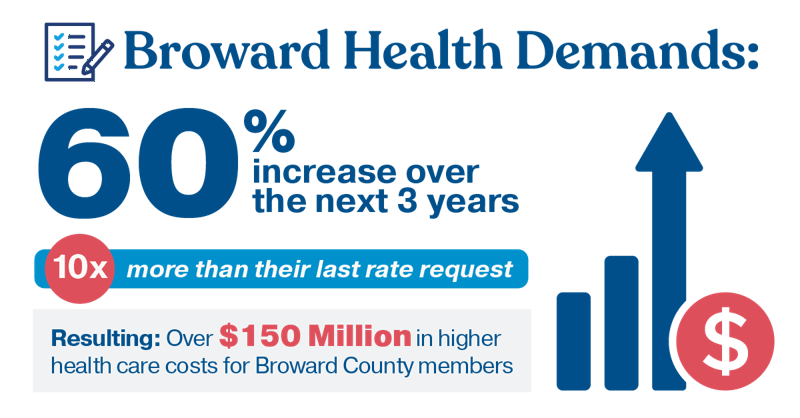
Our goal is to be as transparent as possible, though specific details, including financial discussions, are confidential. What is important to note is that every hospital system is asking for increases, some as high as 30%. We take those requests seriously. Our goal is to reach an agreement that appropriately compensates them and ensures our members have access to quality care at affordable prices.
Broward Health, formally known as the North Broward Hospital District, is a large integrated health system in Broward County. As one of the largest public health systems in the United States, and as a public, tax-payer-funded, and not-for-profit health organization, they have a responsibility to be good stewards of their resources.
Broward Health operates hospitals, urgent care centers, outpatient/ambulatory centers, and other health centers and physician practices across the area.
Florida Blue has enjoyed a more than 30-year longstanding relationship with Broward Health, and we continue negotiating in good faith, as we’ve done from the start and as part of a normal contract renewal process.
When health care systems demand unreasonably large rate hikes, these costs are passed onto members in the form of higher prices for doctor visits and increased premiums. While we want to support the health care systems, it would be irresponsible for Florida Blue to agree to rates that unnecessarily drive-up costs for our customers and members.
We understand that hospitals across Florida and the country are facing tremendous financial pressures. Health plans are also feeling the squeeze, and so are those covered by insurers who depend on these systems for care.
The current economic environment is tough on everyone. That is why, during contract negotiations, Florida Blue acts as an advocate for the businesses and members we serve, working to keep health care costs from rising and placing further strain on the budgets of businesses and households alike.
If you have received care from a provider whose contract may be ending, you will receive a letter from Florida Blue and/or Broward Health, as required by state regulations.
What’s next?
In some cases, members with a chronic condition or in treatment may continue to receive care while paying in-network rates after their provider’s contract ends. This is called Continuity of Care.
Your letter will provide more information on who to contact to learn how you can continue your present course of treatment with your current provider. It will also provide information on how to find a new provider.
If you see a Primary Care Physician (PCP) at Broward Health, the letter you receive will match you to another high-quality local doctor who is in-network. Should you wish to select a different PCP, please contact our customer service teams and we’ll be happy to work with you to choose another doctor.
You may be able to establish continuity of care with your current provider at the current in-network benefit level for a period of time if you are receiving treatment for a covered service or for a complex or chronic medical condition. Such conditions include pregnancy or scheduled nonelective surgery.
There are specific state and federal protections and details on who qualifies for Continuity of Care and the length of time for covered care.
You can contact customer service at the number on the back of your member ID card for more information about this process. Call us anytime and we will help answer any questions you may have or provide clarification.
You can easily find and choose other in-network hospitals, physician, or clinical sites in your area by logging into your member account.
In an emergency, members should always seek care at the closest hospital. Care for an emergency medical condition will be covered as in-network (even if the member doesn’t otherwise have out-of-network benefits), though out-of-pocket costs will vary depending on their health plan benefits.
You are covered for emergency services, even at an out-of-network facility. If you are admitted to the hospital after an ER visit, and the hospital is no longer in the network, you are protected. The hospital stay for the emergency is covered at your in-network cost share. This is because the stay is billed as a single claim and subject to consumer protection from the No Surprises Act. Under the No Surprises Act, you’re also protected from balance billing for emergencies. If you need to return to the out-of-network hospital for non-emergency care, that visit would not be subject to the No Surprises Act. In that case, your out-of-network benefits will apply as outlined in your contract.
If your doctor is leaving our network and you’re pregnant, we'll work with you to ensure you can continue receiving care from them. There are policies in place to protect pregnancy and postpartum care with your current providers and care team.
- For expectant moms with an HMO plan, your care from your provider will be covered by your in-network benefits.
- For those with a PPO plan, you can still use your in-network coverage for 90 days if Broward Health decides to leave the network, and then your care is covered by your out-of-network benefits.
About the provider network
We’re committed to ensuring our members have access to the care they need. Our network includes many providers that share our commitment to high-quality, cost-effective care. This includes high-quality hospitals, doctors, specialists, labs, and facilities in your neighborhood and throughout the area.
A provider network includes the doctors, specialists, hospitals, labs, pharmacies, and other medical professionals that are part of your health plan. We negotiate rates with these providers, so you get high-quality care at the lowest possible prices. Choosing in-network care saves you money.
An in-network provider currently has a contract with Florida Blue, and when you see them, you are typically only responsible for cost shares and deductibles. Because they’ve agreed to prices with your health plan, you pay less when you visit them. It’s like having a member discount card for your health care. We cover more of the costs for in-network providers.
An out-of-network provider does not have a contract with Florida Blue, and you may be responsible for most, if not all, of the bill, including cost shares and deductibles.
Learn more about the types of networks that health plans offer.
Our customer service team can also help you understand the difference between in-network versus out-of-network benefits and more.
About health care costs
There are several factors that affect what you may pay for a visit to a provider. If you see a provider that is not in your network, the amount we pay (the reimbursement rate) may be lower, meaning you will have a larger amount that you must pay out of your pocket.
If you have a plan with a deductible and have not met your annual deductible, you may pay the difference between the negotiated contract rate Florida Blue pays the provider and what is left of the bill.
In general, we are finding that health care systems bill health insurance plans more to make up for the lesser amount they receive for Medicaid and Medicare reimbursements. In other words, employer sponsored health plans subsidize other lower paying types of plans.
Florida Blue is mission-driven to help people and communities achieve better health at a price they can afford. Unlike a for-profit organization — whose goal is making money for investors — we’re helping people and communities achieve better health.
We are required by law to spend at least 80-85 cents (the exact amount varies by plan/product) of every premium dollar directly on the care of members, and we exceed that by putting policyholders’ money where it matters: their health.
The main drivers of rising health care costs are the direct costs of medical care — a combination of prescription drugs and services provided by hospitals, doctors, and medical facilities.
Advocating for access and affordability in these negotiations is our responsibility.
We’re reinvesting our profits to enhance our capabilities and better support the well-being of our members and communities
To learn more
To help educate individual and group members about the contract negotiations process, we have developed informational tools that highlight how we regularly work with doctors, pharmacies, and other health care facilities and providers, advocating in the best interest of the communities we serve.
Negotiations between health insurers and health care providers can be unsettling for members whose access to care may be impacted — this can cause feelings of uncertainty.
Our goal is a resolution, and we will keep you updated on the progress of the negotiations with Broward Health.
We encourage you to reach out to us if you have any questions or concerns about your coverage or whether a particular provider could be affected. Just call the number located on the back of your member ID card.
We're here to support you and want to make sure you have all the information you need.