September 30, 2025
Rising medical costs and economic uncertainty have helped create a complex and shifting time in health care and beyond. For many Americans, health care can be intimidating and unaffordable, with almost one-third of U.S. adults saying they have skipped or postponed getting the care they needed due to the cost.1 These cost challenges are echoed in Florida. More than 60% of Floridians experienced at least one health care affordability burden last year and 80% worry about affording health care in the future.2
In addition to cost challenges, Floridians also face unique obstacles in accessing quality care. More than 1.25 million people live in rural counties in Florida3, where access to health care services can be limited. In addition, with a statewide provider shortage (just an average of 26 physicians per 10,000 people4 and one primary care doctor per 1,370 people5), many Floridians struggle to get the quality care they need. These factors, coupled with a growing population, translate to delayed or avoided care, which can lead to worsening health problems and more costly care down the line.
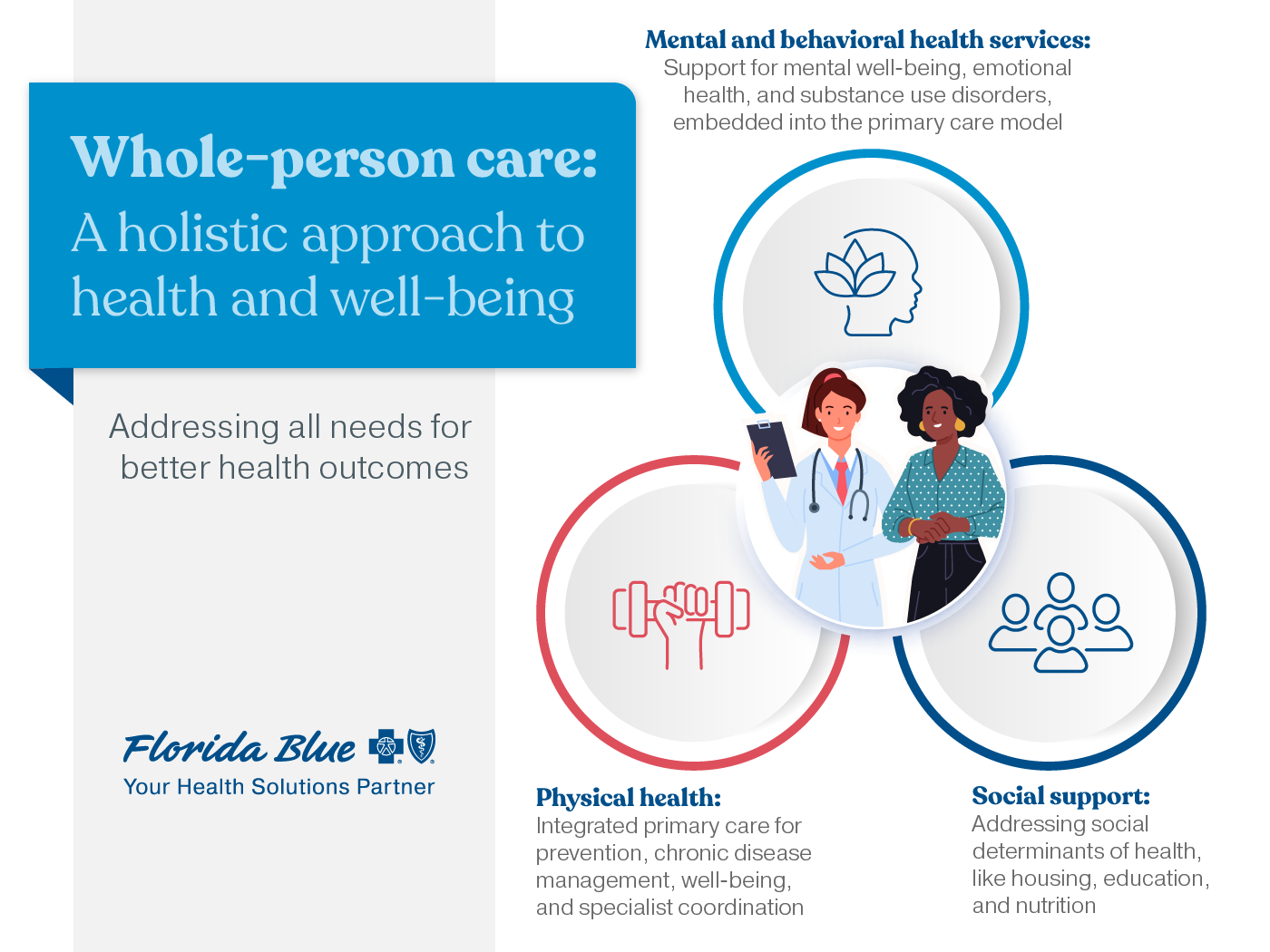
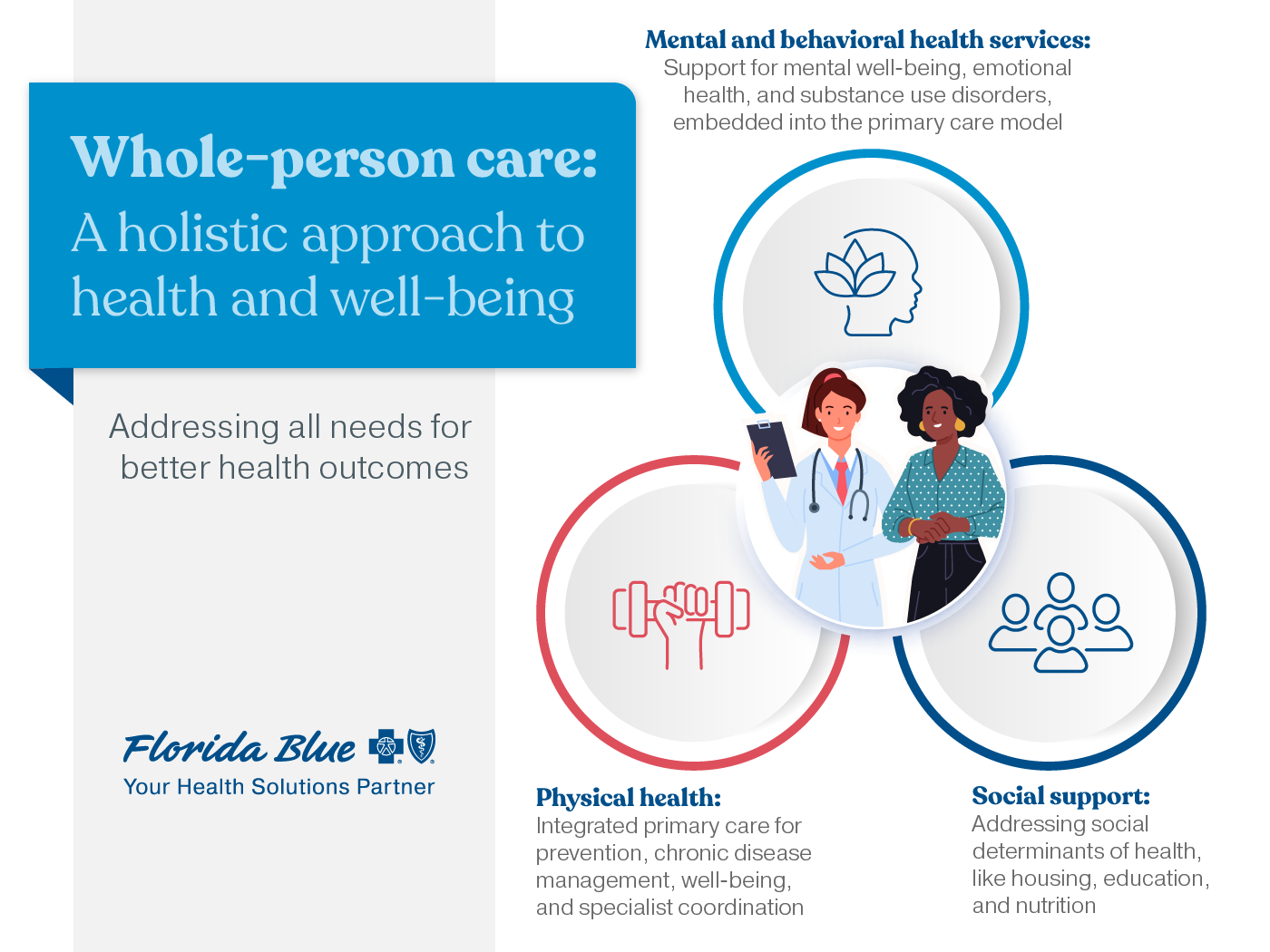
The need for whole-person care
Florida’s health care challenges underscore the need for a more comprehensive approach to care. Traditional care models often focus on treating individual illnesses or conditions. They may not address the underlying social and economic factors contributing to poor health outcomes. Whole-person care, on the other hand, takes a more complete method, recognizing that physical, mental, and emotional health are interconnected, and emphasizes the importance of prevention and early intervention of avoidable and costly conditions.
This also addresses the social determinants of health, those factors outside the health care system, by collaborating with community-based organizations and leveraging their expertise to address the social needs of individuals. For example, Florida Blue works closely with key organizations to invest in our Growing Resilient Communities initiative to break the cycle of generational poverty in some of the most under-resourced communities in Florida. By working together, payers, providers, and community organizations can create a more comprehensive and sustainable approach to health care that goes beyond traditional medical treatment. This collaborative method enables us to identify and address the root causes of poor health outcomes, provide support and resources to individuals, and ultimately improve the overall well-being of our communities.
Making care easier and more accessible
Making care easier and more accessible is at the heart of Florida Blue’s mission to help people and communities achieve better health. One of the challenges is the traditional fee-for-service model, which can exacerbate fragmented care delivery and does little to align care coordination. This can lead to a complex and confusing system for patients, who are often left to navigate multiple providers and payers on their own. We're committed to changing that by putting the whole person at the center of our care model, addressing their physical, mental, and social needs to achieve better health outcomes and improve their overall well-being.
Florida Blue’s approach
At Florida Blue, we believe that by focusing on the whole person, rather than just their symptoms, we can create a more patient-centered and sustainable health care system. To achieve this vision, we collaborate with hospitals, doctors, and community organizations to create a more seamless and coordinated care experience for our members.
For example, earlier this year, additional Florida Blue | Sanitas Medical Centers opened, supporting our membership growth across the state. Each Center has Sanitas care teams that provide personalized, comprehensive care that treats the whole person, not just a condition or injury. The innovative Sanitas care model puts the patient at the center of everything their care team does, including assessing physical, emotional, and social needs; developing personalized care and wellness plans; coordinating care and wellness activities, including specialist referrals; and providing social support and connections to community resources.
Value-based care models, like the one Sanitas uses, lead to enhanced patient experience and increased satisfaction. They also lead to fewer ER visits, reducing preventable hospitalizations.6
Florida Blue also recognizes the importance of prevention in maintaining overall health and well-being. Regular check-ups and exams can help detect serious diseases early, which can be lifesaving. That’s why for most of our Florida Blue health plans, we offer routine checkups, vaccinations, and mental health support to members at little to no extra cost.
Supporting mental health and well-being
We also believe that there’s no health without mental health, so our whole-person care approach includes addressing mental health and well-being. To support this, we've established common definitions of well-being that guide our integration of behavioral and mental health into our care models. This is an example of how delivering personalized care considers factors beyond the health care system. Defining mental well-being also helps with making our members and the public aware, creating relationships with like-minded clinical and community organizations, and provides a better way to evaluate outcomes at the individual level and across populations.
We've been a leader in integrating mental health and well-being into our care models in a variety of ways. For example, at Sanitas and FHCP, their programs embed general mental health care and supports those struggling with substance use disorders. Both programs operate within the primary care setting and aim to intervene early, bridge gaps, and foster healthy lifestyles. Additionally, we were one of the first insurers to include a mental health metric in our contracts with primary care providers, to drive accountability which increases access and quality over time.
Florida Blue members also can find help with our behavioral health care partner, Lucet. They connect eligible members to mental health clinicians that are right for them in as little as two weeks. In 2024, 1,000 mental health providers were added to Lucet’s scheduling technology, dramatically shortening the wait to see a provider and 72% of members who used the online scheduling tool kept their appointments.7
Looking to the future of health care
In the future, we envision a health care system that is more hyperlocal, with a curated network of doctors and health care providers who are committed to delivering high-quality, affordable care. By building intentional relationships with local health care providers and community-based organizations, we can create a more seamless and coordinated care experience for our members, helping all aspects of their health and well-being, while improving the provider experience. This approach will not only improve health outcomes, but also make health care more accessible and affordable for everyone.
Health care can no longer be just about treating illnesses; it must be about preventing them, managing chronic diseases, and supporting mental health and well-being. By putting people at the center of everything we do, we can personalize care that meets individuals where they are in their health journey and support them in achieving their unique health goals.
At Florida Blue, we’re committed to making whole-person care a reality, not just a buzzword. We believe that by working together, we can create a health care system that truly supports the well-being of all those we serve.
1 KFF. American’s Challenges with Health Care Costs.
2 Healthcare Value Hub. Florida Residents Struggle to Afford High Health Care Costs.
3 Florida Health Department. Florida’s Rural Counties
4 Florida Health Department. Florida Physician Workforce.
5 Count Health Ranking & Roadmaps. Florida data: Primary Care Physicians.
6 Analysis of calendar year 2023 value-based provider performance versus non-value-based providers prepared by Florida Blue in 2024. Included in From volume to value: The shift in health care that’s helping put patients first.
7 Reported in the 2024 GuideWell Impact Report.